We are here to assist you with your insurance inquiry or complaint about a health, life, auto or homeowners insurance policy. Additionally, we are here to assist you if you have a complaint involving an insurance producer, public adjuster or adviser. That's what Beighley did when he was involved in a case involving an out-of-network claim for a health care provider. He notes that some insurance companies have appeal options buried on their websites. For example, here's the appeal process for Arkansas BlueCross BlueShield.
How To Report An Insurance Company In Florida Your appeal should include the member name, health plan ID number, a reference number for the claim being appealed , and date and provider of service. And you must file an appeal within 180 days after you have been notified of the denial of benefits. The Utah Insurance Department has a staff of insurance experts available to help you understand your insurance coverage and answer your questions. If you have been unable to resolve a problem with your insurance company or agent, you may contact our staff for assistance, or file a written complaint. If your complaint involves health care insurance, please refer to the HEALTH CARE INSURANCE COMPLAINTS section below. All complaints and information requests are reviewed upon receipt to ensure that they are within the jurisdiction of the DOI.
The respondent will receive written notification that a complaint has been filed along with a copy of your complaint and the supporting documentation. The respondent has 30 days to provide a written response to the complaint. The complaint is then assigned to a CSU examiner for review.
A complaint to your state's insurance department may accomplish multiple things. First, the insurer's claims department will know that there's someone who will do what's necessary to get a reasonable settlement. That alone may encourage the company to re-evaluate your claim and arrive at a fairer offer. Additionally, because formal complaints create additional work for insurers, they'll make more of an effort to settle.
With help from the state insurance department's investigative team and your public adjuster, you're more likely to get the settlement you deserve. INDEPENDENT REVIEW. If you have had a claim denied by a health insurance company and have completed the appeal process outlined in your policy, you may be eligible for an independent review. For information regarding Independent Review of an Adverse Benefit Determination click here.
Health Care Provider ComplaintsDIFS regulates the business of insurance transacted in Michigan. DIFS accepts complaints from parties involved in the contract, such as the insured, policyholder, or certificate holder. Because a health care provider is usually not a party to the health plan, DIFS generally does not accept complaints from providers.
Please be sure to send us all relevant information when you submit your complaint. If you need to send more documents or a longer summary than the form allows, please email the information to and note that you filed a complaint and are providing additional documentation. Please be aware that Consumer Services will send a copy of your complaint and any related materials to any company, agent or licensee involved in this matter.Please do not send any medical records.
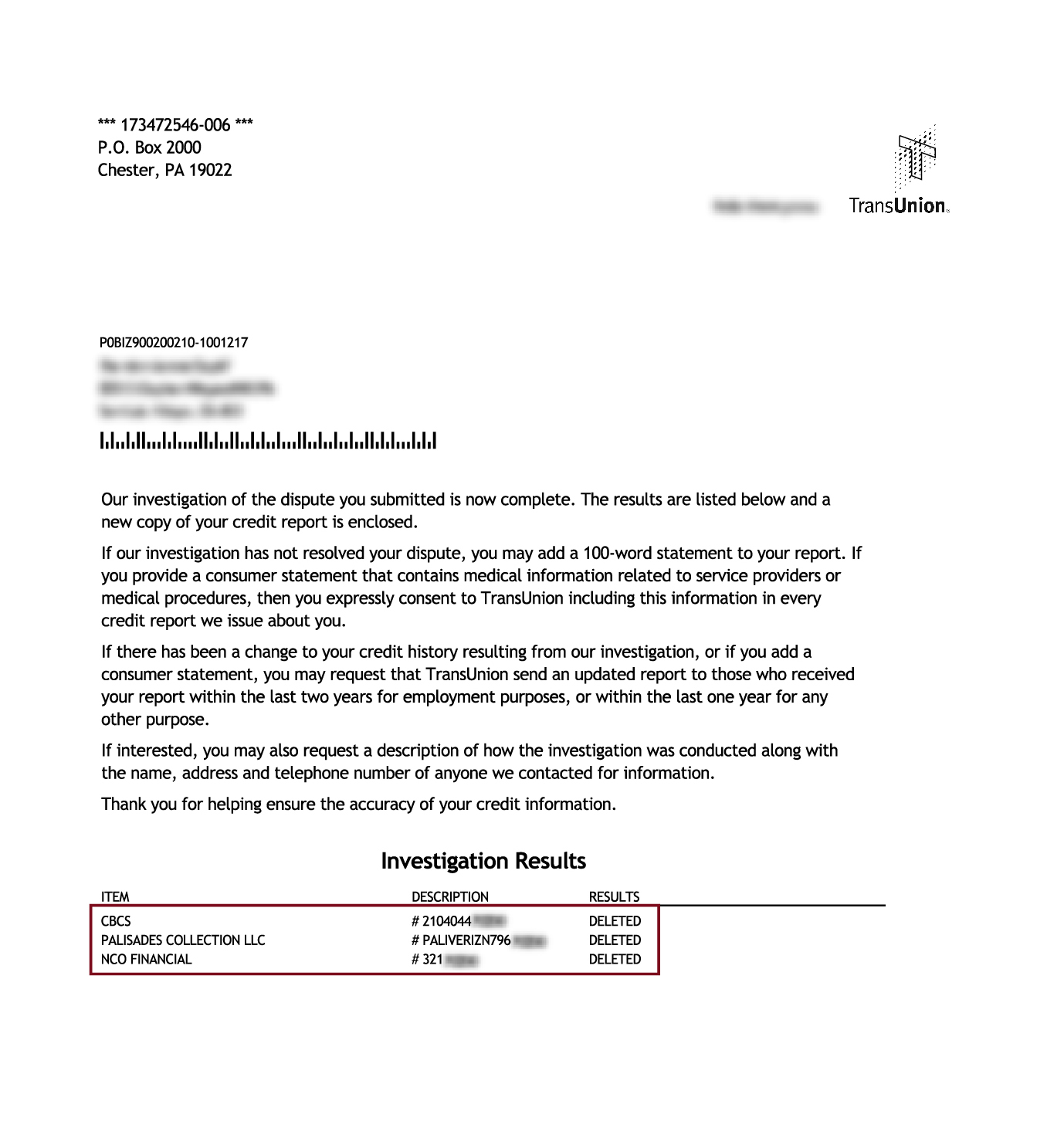
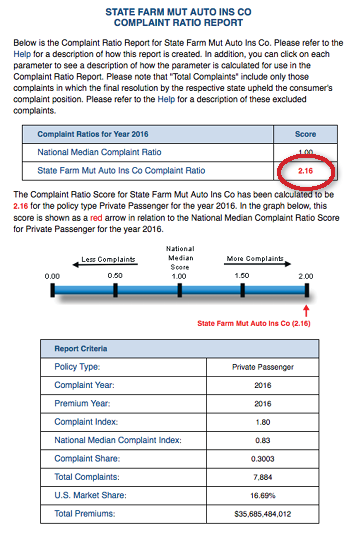
Every day, we trust our insurance companies to represent our best interests in a forthright and honest manner. Unfortunately, sometimes insurance agents or companies fall below this standard. As a consumer, you have the right to file a complaint and report your insurance company if you feel that you have been treated unfairly. Read on to learn more about how to report an insurance company for wrongdoing. The number of complaints to your state's department of insurance is a matter of public record. It shows how many consumers have purchased a policy, how much the policies are written for, and the number of complaints.
The department then divides the number of complaints by the policies written and calculates a complaint ratio. The higher the complaint ratio, the worse the insurance company. DIFS will accept complaints from providers having problems with receiving timely payment for submitted claims without any errors or other issues. These claims are referred to as "clean claims" and must be paid within 45 days after it is received by the health plan. For more information on clean claims and to obtain the Clean Claim Report form, visit /DIFS.
If you are unable to file a complaint on the online portal, please select the applicable form below to submit a complaint by mail or fax . Provide as much information as possible, attach copies of all supporting documentation to the completed complaint form, and keep the original documents for your records. The Division of Insurance Consumer Services sections investigate individual consumer complaints against insurers.
Investigations may result in financial recoveries for consumers in the form of additional claim payments, overturned denials of policy benefits or other refunds for the consumer. Investigations can also result in policies being reinstated for consumers. If this is your first time using the Provider Complain Form you will need to create a portal account, then follow the prompts in Ask for Apps to request access to Provider Complaint Forms. The Department works to ensure all insurance companies, HMOs, producers selling insurance in Illinois and other regulated entities obey state insurance laws.
The Department provides consumer information and investigates complaints about companies and producers. Before you file a request for assistance with the Alabama Department of Insurance, you should first contact the insurance company or producer in an effort to resolve the issue. If you do not receive a satisfactory response, then fill in the Online Consumer Complaint Form. The speed and quality of the state insurance department's response may vary according to your location. If you are a medical provider looking to file a complaint against a health insurance company? Please visit the Procedures for Submission of Complaints by Providers Against Insurersbefore submitting.
Complaints are filed through the Consumer Portal, where you will first need to create an account using an email account and password. The portal is a secure way for consumers to submit insurance complaints and communicate with the Division of Insurance. Once the account is created, you will use the email and password to log into the Consumer Portal. The Consumer Services Division is the investigative arm of OCI. Our job is to ensure fair and equitable dealings between insurers, agents, and policyholders. If you have a complaint about your insurance provider or agent, or how a claim is being handled, we may be able to help you resolve the issue.
The Division of Consumer Services is happy to assist you with your insurance questions and concerns or open a formal complaint. Our dedicated and experienced helpline specialists are continuously trained and informed about any changes that occur to the 26 different categories of insurance they confront on a daily basis. We are ready to contact the insurance company on your behalf to assist you with your insurance complaint.
Regardless of what it's called, your state's insurance agency website will have information about how to file a complaint against an insurance company. In many cases, consumers are able to file claims online through the governing agency website. The National Association of Insurance Commissioners has a helpful interactive map that can help your state's insurance agency website. If there's no complaint form, your letter should include the accident date, names of those involved, a description of the claim, the claim number, and an explanation of the difficulties posed by the insurance adjuster.
It's important to document conversations with adjusters, both public and private, and to keep copies of all correspondence so the insurance department's investigative team will know the basis for the complaint. If the situation calls for a formal insurance complaint, simply mentioning it to the adjuster may encourage them to make a fair settlement offer for your property damage claim. Although the state insurance board isn't likely to become involved, their adjusters would prefer to avoid complaints if possible. Excessive complaints can bring department inquiries, and adjusters don't want to have such complaints on their records. However, when you have a Public Adjuster on your side, you're more likely to receive a fair offer and less likely to file a complaint. All states have agencies overseeing the insurance business, and each agency has a complaint division that gets involved when claimants have trouble with insurers.
It's quite rare for the agency to intervene in individual claims, but in this guide, we'll explain how and when to file a formal complaint. If the issue cannot be resolved with the insurance company, we encourage you to file your complaint online using our customer portal. Find information about regulatory actions, violations, and complaints that others have filed against financial service providers, investment brokers, and insurance companies. In these cases, the Insurance Department does not have jurisdiction to assist you with a complaint. For information regarding Self-Funded Health Insurance Claims click here. Review your file to determine if the insurance company, HMO, insurance agent, or adjuster violated state insurance laws.
Use our online Consumer Complaint Formto file a complaint with DFS about an insurance company, vacant property, student loan, mortgage, foreclosure, bail agent, bank, lender, or other financial service or product. You can also check the status of a complaint, or add information, such as a Letter of Authorization , to an existing complaint. Be aware that we may share a copy of your complaint with the company or individual you are complaining about. One of our most important jobs is to help educate North Carolinians about insurance-related issues so you can make informed decisions for you and your family.
If you have questions about insurance, need to file a complaint or want to report suspected insurance fraud, we can help. We urge all consumers who are having trouble to first try to resolve any problems with their insurance company or agent. When creating your account it is important to MAKE NOTE OF THE PASSWORD you select, it will be required to access the status of your complaint.
Once your account has been created, you will be able to access the complaint form and submit your complaint. The purpose of a password-protected account is to provide secure transmission of the complaint and communication to and from the Insurance Department. If you have multiple complaints about the same carrier, please provide a representative sample of no more than ten claims.
Include the date of service, date of submission, how it was submitted , date of response/remittance advice from the carrier, and a copy of the claim form and member identification card, if available. If additional information was requested by the carrier, include the claim number and the date of re-submission. If you have a complaint about an insurance company or claim, we can help.
Find out more about the types of insurance complaints we deal with, and what we can do to help put things right. Also, if your insurance company begins including its legal representation in the conversation, you may want to consider retaining your own attorney. It's always important to be aware of any applicable statutes of limitation for your claim, which, if missed, may cost you the right to file a lawsuit. For this reason, you may want to consider contacting an insurance law lawyer in your area to learn more. Provincial and territorial insurance regulators oversee the licensing and conduct of insurance agents and brokers. Each province and territory has its own insurance regulator and all insurance companies must follow the rules and regulations of the province or territory in which they carry out business.
The first step is to find out whether there's a specific complaint form and where to send it. It's easy to find the state insurance department's phone number, form, and website with a quick Google search. Your complaint along with a letter from the IDOI is mailed to the insurance company the complaint is against.
By Indiana law, the insurance company has 20 business days to respond in writing back to the IDOI. Virtual Viewing RoomThis virtual viewing room allows you to see insurance company rate filings, examination reports, and related information. Self-insured employers and health and welfare benefit plans – Many large employers provide health benefits for their employees through self-insured plans. Although self-insured plans are frequently administered by an insurance company, the employer bears the risk for paying claims.
Federal law exempts self-insured employer plans from state insurance regulation. The same is true of health and welfare benefit plans (i.e., union plans). Consumer Services responds to consumer inquiries and intervenes on behalf of consumers to resolve complaints against insurers, agents, and other licensees.
Consumer Insurance Search Find information about insurance company complaints, licenses and financial health. Every state has a department of insurance that regulates insurance companies and agents. The various agencies are known by different names around the country. For example, in California the governing insurance agency is the Department of Insurance, while the state of Hawaii regulates insurance through the Department of Commerce and Consumer Affairs. Complaints to a state insurance department aren't guaranteed to work. In Ohio, the department of insurance explicitly says it will not force a company to satisfy you if no laws have been broken, even if you believe the company or agent has not been fair.
If the ombudsman approach doesn't work, you can also consider taking your complaint public. A plea for help on social media may get your insurance company's attention. Insurance companies have an appeal process that you should follow before you call for outside help. While your insurance company may not volunteer information about the appeals process, you should ask about it before filing a complaint to an outside party.
She filed a complaint with her insurance company's appeals department which is overseen by a third party because it is operated by the government. She found the names of the insurance company's board of directors and executives and sent a polite appeal to them. Our office provides an independent, objective, efficient and free service to policyholders and others in respect of their complaints arising from long-term insurance policies. The insurance company must reply to the issues addressed in the Consumer Complaint and respond to the Division within 28 calendar days. The Consumer Services Section of the Nevada Division of Insurance handles all requests for consumer assistance. We can help you understand your policy and answer any questions you might have regarding claims or companies.
Your identity and any personally identifiable information and personal health information will remain confidential subject to state and federal laws. However, in order to help resolve your complaint, a copy of the complaint will be sent to the appropriate company/agent for a response. You may also file a complaint online via our secure consumer portal or by e-mail to Maryland law gives Maryland consumers the right to appeal a decision that denies you coverage for medically necessary treatment. If your doctor has determined that certain medical treatment is needed, but your HMO or health insurer does not agree, this law allows you to appeal. Generally, you must file a grievance with the carrier first before you can file a complaint wit the MIA.
In some cases, though, including, for example, when you have a compelling reason, you can file a complaint with the MIA first. For the duration of the COVID-19 state of emergency, we are asking all consumers to use the online portal to file complaints, if possible. You may file a complaint with us if you are unable to resolve your dispute with the insurance company or aren't satisfied with how they responded to your claim. Some companies that appear to be acting as insurers are not authorized to write insurance in Texas. Be very suspicious of coverage that seems too good to be true or rates far below what other insurance companies are quoting.
























No comments:
Post a Comment
Note: Only a member of this blog may post a comment.